Standard Dental Implants
What are Standard Dental Implants?
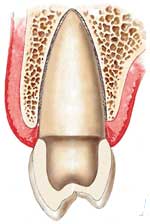
A dental implant is really a very simple metal screw which is designed to thread into the bone of the jaw and to allow for the attachment of a (prosthetic) tooth at the top. Implants are made of Medical grade Titanium or Titanium Alloy. Your dentist will purchase the implants in sterile packaging and place them in a small hole in the bone which he or she has prepared as part of the implant placement procedure. The bone will fuse to the implant over a short period of time in a process referred to as 'osseointegration' and once this process is successfully completed (3 to 6 months) the implant is permanently in place.
Types of Implant
- Single tooth replacement
- Multiple tooth replacement
- Denture Stabilization
Single tooth replacement
A single Implant is used to replace a single tooth, can be used both in the front of the mouth and the back of the mouth
Central Incisor :


Lateral Incisor:


Back Molar:


Multiple tooth Replacement:
Can be used to replace teeth in the form of a Bridge ( teeth joined together ) or with multiple individual teeth
Two Molars and a Premolar:



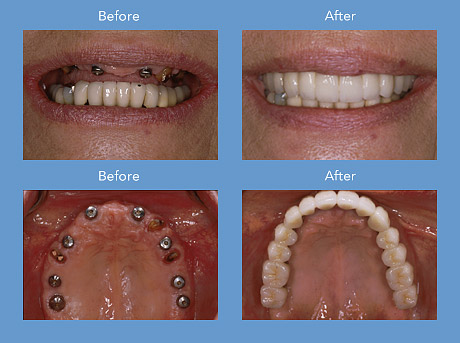
Full mouth replacement:
Replacing upper teeth with a fixed Porcelain Bridge



Replacing upper teeth with a fixed Porcelain Bridge
Denture Stabilization:
Denture Clicks in and out using precision attachments on at least two Implants




Strong, durable, and natural in appearance, implants are among the most successful dental procedures performed. Although you have a number of restorative options for the treatment of missing teeth, none has proven to be as functionally effective and esthetically natural as implants. In many cases, dental implants may be the only logical choice for the restoration of all necessary functionality of the teeth and supporting structures.
Advantages of Implant Dentistry
Dental implants are stronger, more durable, and more natural than their restorative counterparts (bridges and dentures). Implants offer a permanent solution to tooth loss.
- More attractive appearance.
- Great comfort.
- Don't need to drill into the teeth on either side.
- Helps prevent bone loss due to tooth removal.
- Greater ability to chew food.
- No rubbing, clacking, or pain.
- No cream or adhesives.
- Not having to take out at night.
- Not overnight soaking in a glass.
1. Initial Consultation
The Implant process needs three people; The Surgeon to place the
Implant, the Dental technician to make the tooth and the Dentist to
connect the tooth to the Implant and oversee the process. The first
step is an examination and consultation. This usually involves x-rays
and may include taking impressions for models of your teeth. If you
have already lost a significant amount of bone, additional x-rays taken
at another facility that specializes in this type of x-ray may also be
recommended. During the examination, we will be evaluating the area(s)
of your mouth where teeth are missing, including the amount of bone
available to support the placement of implants. we will also be
evaluating the type of replacement teeth that will best meet your
needs. A review of your health history will indicate whether there are
any medical conditions that could prevent you from being a candidate
for implant treatment.
2. Dental Implant Placement Procedure
The dental implants are placed in the bone using a gentle surgical
technique. The Surgeon places a small-diameter hole (pilot hole) at
edentulous (where there is no tooth) jaw sites in order to guide the
titanium screw that holds a dental implant in place. To avoid damaging
vital jaw and face structures like the inferior alveolar nerve and the
mandible (lower jaw), a Surgeon must use great skill and expertise.
After the initial pilot hole has been drilled into the appropriate jaw
site, it is slowly widened to allow for placement of the implant screw.
Following this placement, a protective cover screw is placed on top to
allow the implant site to heal and the dental implant to anchor
(osseointegration).
3. Abutment Attachment Procedure
Following the appropriate bone remodeling period, a small connector post
called an abutment is attached to each dental implant. The permanent
replacement teeth will eventually be attached to the abutments.
4. Fabrication of Replacement Teeth
A series of appointments will be needed to take impressions of your teeth
and the implant abutments; place temporary replacement teeth; select the
appropriate shade for your replacement teeth and try them for proper fit. In
between these appointments, the laboratory technician will fabricate your
replacement teeth and the underlying structures that will be attached to the
dental implants.
5. Completion of Dental Implants
Once the above phases are complete, then your new dental implants will be
fixed to the abutment and you'll have a beautiful new set of teeth that
look, feel and function just like the real thing.
6. Ongoing After Care
Regular examinations will be necessary to monitor and maintain you
Implants to ensure that any problems are caught early, this will help
ensure the best chance for longevity
Today's dental implants are virtually indistinguishable from other teeth. This appearance is aided in part by the structural and functional connection between the dental implant and the living bone. Implants are typically placed in a single sitting but require a period of osseointegration.
Osseointegration is the process by which direct anchorage of a dental implant root and the bone of the jaw occurs. Osseointegrated implants are the most commonly used and successful type of dental implant. An osseointegrated implant takes anywhere from three to six months to anchor and heal, at which point your dentist can complete the implant procedure. Once the implant has anchored with the jawbone, an artificial prosthesis (tooth) may be attached and the process is done. If osseointegration does not occur, the implant will fail. Detailed procedural steps are as follows:
What are the Risks?
- In rare circumstances Implants have been known to fail and they will have to be removed through a subsequent procedure. ( usually just unwinding them by hand )
- It is possible that implant superstructure may fracture during the implant’s life cycle, and in the event a fracture were to occur, the fractured implant may be removed or left in the jaw if its causing no problem, determined by professional judgment.
- If the patient keep good oral hygiene and does not return for return for appropriate post-operative care including plaque removal, Implants can fail.
- The use of tobacco, including cigarette smoking as well as excessive alcohol consumption can cause failure of the dental implants.
- Swelling, infection, bleeding and/or pain may be associated with any surgical procedure, including Implants and the said conditions may occur during the life of the implants.
- Temporary or permanent numbness may occur in my tongue, lip(s), chin, or jaws as a result of this procedure as well as the possibility of sinus involvement in my upper jaw. Although cases occurring with Mini Implants are extremely rare
Does the Procedure Hurt?
It is often done under local anesthesia and patients generally experience some discomfort after the procedure although this is usually controlled by paracetamol. It is similar to having a simple tooth extraction.
Success Rates of Dental Implants
Studies have shown a five-year success rate of 95% for lower jaw implants and 90% for upper jaw implants. Many other studies have shown 5 year success rates in the high nineties.
Failure of a dental implant is often related to failure to osseointegrate correctly. A dental implant is considered to be a failure if it is lost, mobile or shows peri-implant (around the implant) bone loss of greater than 1.0 mm in the first year and greater than 0.2mm a year after.
Dental implants are not susceptible to dental caries but they can develop a condition called peri-implantitis. This is an inflammatory condition of the mucosa and/or bone around the implant which may result in bone loss and eventual loss of the implant. The condition is usually, but not always, associated with a chronic infection. Peri-implantitis is more likely to occur in heavy smokers, patients with diabetes, patients with poor oral hygiene and cases where the mucosa around the implant is thin.
Currently there is no universal agreement on the best treatment for peri-implantitis. The condition and its causes is still poorly understood.
Risk of failure is increased in smokers. For this reason implants are frequently placed only after a patient has stopped smoking as the treatment is very expensive. More rarely, an implant may fail because of poor positioning at the time of surgery, or may be overloaded initially causing failure to integrate. If smoking and positioning problems exist prior to implant surgery, clinicians often advise patients that a bridge or partial denture rather than an implant may be a better solution.
Failure may also occur independently of the causes outlined above. Implants like any other object suffers from wear and tear. If the implants in question are replacing commonly used teeth, then these may suffer from wear and tear and after years may crack and break up. This is a very rare occurrence, however possible. The only way to minimize the risk of this happening is to visit your dentist for regular reviews.
In the majority of cases where an implant fails to integrate with the bone and is rejected by the body the cause is unknown. This may occur in around 5% of cases. To this day we still do not know why bone will integrate with titanium dental implants and why it does not reject the material as a 'foreign body'. Many theories have been postulated over the last five decades. A recent theory argues that rather than being an active biological tissue response, the integration of bone with an implant is the lack of a negative tissue response. In other word for unknown reasons the usual response of the body to reject foreign objects implanted into it does not function correctly with titanium implants. It has further been postulated that an implant rejection occurs in patients whose bone tissues actually react as they naturally should with the 'foreign body' and reject the implant in the same manner that would occur with most other implanted materials.
Implant Dentistry: New Procedural StrategiesExperienced implantologists have begun to use a new strategy for the replacement of missing teeth. Dental implants are placed into locations where teeth have recently been extracted. When successful, this new strategy can shed months off of the treatment time associated with dental implants because osseointegration is sped up. Candidacy for this type of early intervention is dependant upon anatomical factors of the extracted tooth site. For example, in many cases the extracted tooth site is wider than the implant, making it impossible to place the implant into the site immediately after extraction. Dental work would have to be performed first in order to create a perfect fit for the implant.
Another strategy for implant placement within narrow spaces is the incorporation of the mini-implant. Mini-implants may be used for small teeth and incisors. Get more information about alternatives to traditional implants by checking out our mini implant section.
For more information about Dental implants see Wellingtons leading Dental Implant Dentist here
For more information - Click here>